Breast reconstruction with mesh implants
In Germany, around 70 percent of all breast cancer therapies do not require a mastectomy, but in the remaining 30 percent it is necessary to remove the patients’ breast. These patients are faced with the difficult question of how to deal with this physical change.
At this point, in-depth counseling and information for the patients through the physician is indispensable, as the decisions frequently have to be made under (supposed) time pressure and the patients are very often mentally unable to absorb all the necessary information.
For this reason, in a patient-centered discussion, the patient should receive counseling on all possible procedures (and not only on those offered by the attending clinic), the potential outcomes, risks, and alternatives. In addition, the patient should be informed of her right to get a second opinion. Only this will enable the patient to make an optimal decision for her own situation.1,2
In what cases is breast reconstruction possible?
Reconstruction is generally possible in nearly all cases. The right moment, the appropriate method and the outcome of the reconstruction, however, are very individual, and vary from one patient to another.
What is the best time for reconstructive surgery?
There is no general answer to this question – it has to be discussed individually in every case. In general, it can be said that reconstructive surgery should not cause a delay in adjuvant therapy.2
Primary or secondary reconstruction
Whether primary (single-stage) reconstruction or secondary (two-stage) reconstruction is expedient depends on the indication, the patient’s general situation and her wishes.
Primary reconstruction spares the patient a second surgical procedure. In addition, it helps decrease the patient’s mental stress, as she does not see herself without a breast.
If subsequent radiotherapy is planned, secondary reconstruction may be expedient to prevent a possible impact of the radiotherapy on the reconstructed breast (the implant or the tissue).
Even if skin-sparing mastectomy is not possible and reconstruction with the patient’s own tissue is not wanted, there is hardly an alternative to secondary reconstruction. In this case, after the mastectomy the skin has to be slowly stretched by means of a tissue expander until it suffices for a reconstruction.
Reconstructive procedures
A distinction can essentially be made between two procedures. The breast can either be completely reconstructed using endogenous tissue, or artificial implants can be used. It is also possible to use a combination of these two procedures.
Wherever possible, the surgical technique that is least stressful for the patient and that offers a stable, long-term and aesthetically pleasing outcome should be chosen.2
If the reconstructive surgery is performed after radiotherapy, preference should be given to reconstruction using endogenous tissue. Radiotherapy usually affects the tissue so that it can no longer be stretched and formed as before, leading to difficulties in positioning an implant. If a tissue expander was already implanted prior to the radiotherapy, it should be filled completely and monitored for some time before deciding whether a prosthesis can be implanted or whether reconstruction using endogenous tissue is a better option.1
Breast reconstruction with an implant
Procedure for breast reconstruction with an implant
Implants are generally silicone shells that are filled with silicone or with saline solution. They are available in different sizes and shapes. A breast implant can be positioned both prepectorally (onto the pectoral muscle) and subpectorally (below the pectoral muscle).
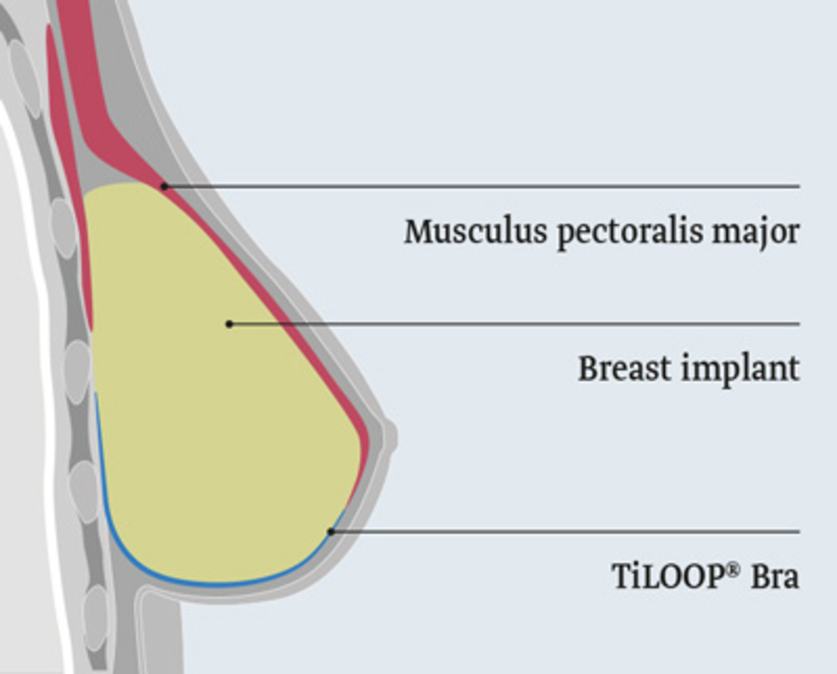
Subpectoral implantation
In this procedure, the pectoral muscle is cut and the implant is positioned below the muscle. Because the muscle is usually not long enough to completely cover the implant and thus to fix it in place, the muscle is usually lengthened. This is done either by means of a mesh implant (e.g. TilOOP® Bra) or an acellular dermal matrix (ADM).
The advantage of this positioning method is that the implant is held in place by the muscle and cannot move.
The disadvantage is that the separation of the pectoral muscle restricts the patient’s shoulder function. It is also associated with a painful healing process. In addition, the pectoral muscle can still contract and thus change the position of the implant.
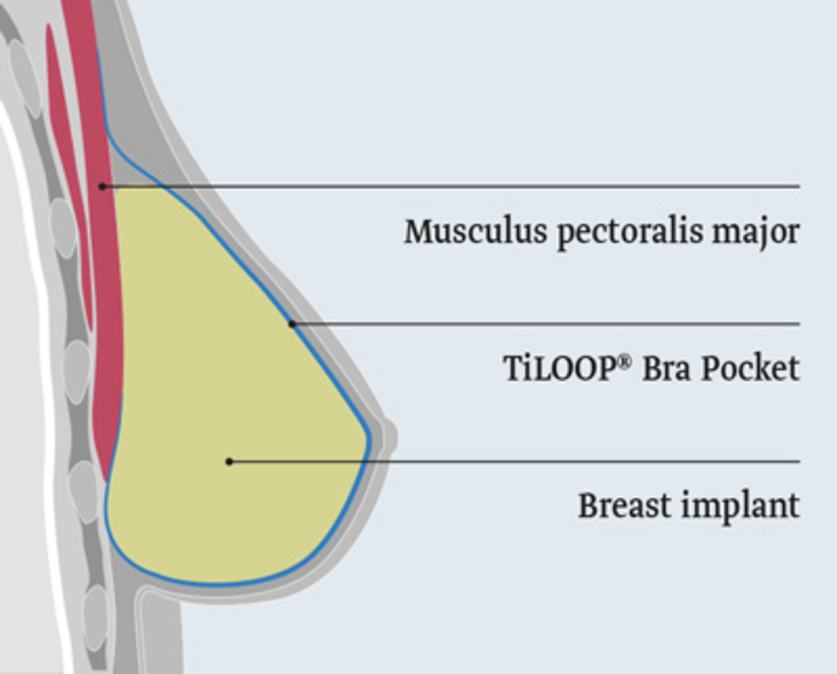
Prepectoral implantation
In this procedure, the implant is placed onto the pectoral muscle and fixed to the pectoral muscle by a mesh implant (e.g. TiLOOP® Bra Pocket) or an ADM.
The advantage of this is that the pectoral muscle does not have to be cut, which significantly decreases the surgical time. It also means that the muscle cannot move, and that the patient’s shoulder function is preserved.
Advantages of breast reconstruction with an implant
- Mastectomy and reconstruction can usually be performed in one surgical procedure
- Short surgical time
- Fewer scars
Disadvantages and possible complications of breast reconstruction with an implant
- No feeling in the breast
- In the event of severe capsular fibrosis, the breast implant has to be replaced
- Sometimes, corrective surgery of the healthy breast is necessary to restore the symmetry
Breast reconstruction with endogenous tissue (tissue flap surgery)
Procedures for breast reconstruction with endogenous tissue
There are different methods for reconstructive surgery with endogenous tissue.
LAT-Flap
The latissimus dorsi (LAT) flap is removed from the back between the shoulder blade and wing of ilium (skin, adipose and muscle tissue) and moved to the front to the breast through a subcutaneous tunnel without interrupting the blood supply. Over time, the smaller surrounding back muscles take over the function of the missing part of the latissimus dorsi muscle, which means that the patient’s mobility and strength are usually not significantly impaired.
TRAM-Flap
The transversus rectus abdominis musculocutaneous (TRAM) flap is removed from between the navel and pubic bone (skin, adipose and muscle tissue) and moved from there to the breast subcutaneously through a tunnel without interrupting the blood supply.
DIEP-Flap
The deep inferior epigastric artery perforator (DIEP) flap is removed from between the navel and pubic bone. Here, only skin and adipose tissue are removed; the abdominal muscle remains intact. The tissue is separated from the blood supply and reconnected to the vessels of the internal thoracic artery in the breast. In order to access these vessels, a small part of the third rib has to be removed.
S-GAP-Flap/I-GAP-Flap
The superior gluteal artery perforator (S-GAP) flap and the inferior gluteal artery perforator (I-GAP) flap are removed from the buttocks area and are comprised of only skin and adipose tissue. The tissue is separated from the blood supply and reconnected to the vessels in the breast.
Advantages of breast reconstruction with endogenous tissue
- Authentic feeling in the breast
- Low risk of rejection
- No capsular fibrosis
- The breast tissue ages simultaneously, which means that the reconstructed breast develops in the same way as the healthy breast.
- The reconstructed breast lasts a lifetime.
Disadvantages and possible complications of breast reconstruction with endogenous tissue
- Microsurgical procedures require a lot of time and personnel
- Complex procedure with larger wounds also in other body parts
- Complex postoperative monitoring
- Longer convalescenceConvalescence (from the Latin "reconvalescere" - becoming strong again) means healing or recovery.
- Higher rate of secondary surgery
- Radiotherapy prior to reconstruction increases the rate of vascular complications
Breast reconstruction with autologous fat
Procedure for breast reconstruction with autologous fat
In reconstruction with autologous fat (lipofilling), adipose tissue cells are aspirated from the patient (for example, from the abdomen, hips or thighs), prepared and injected into the breast.
Advantages of breast reconstruction with autologous fat
- No major surgery required
Disadvantages and possible complications of breast reconstruction with autologous fat
- No long-term experience available yet, in particular with regard to the impact on cancer cells possibly still present in the body
- Interdisziplinäre S3-Leitlinie für die Diagnostik, Therapie und Nachsorge des Mammakarzinoms, Langversion 3.0, Aktualisierung 2012 AWMF-Register-Nummer: 032 – 045OL
- AGO, Empfehlungen gynäkologische Onkologie Kommission Mamma, Onkoplastische und rekonstruktive Mammachirurgie
Expert interview

Dr. Donato Casella talks about breast reconstruction with mesh implant.
Contact
You have questions regarding titanised mesh implants? Please use our contact form.
Surgery-Workshops
Here you can find more information about our surgery workshops.
